You are viewing this post: Chronic Exertional Compartment Syndrome – Everything You Need To Know – Dr. Nabil Ebraheim | ภาวะ compartment syndrome
Table of Contents
Chronic Exertional Compartment Syndrome – Everything You Need To Know – Dr. Nabil Ebraheim
นอกจากการดูบทความนี้แล้ว คุณยังสามารถดูข้อมูลที่เป็นประโยชน์อื่นๆ อีกมากมายที่เราให้ไว้ที่นี่: ดูความรู้เพิ่มเติมที่นี่
Dr. Ebraheim’s educational animated video describes the condition of chronic exertional compartment syndrome in the lower leg.
Follow me on twitter:
https://twitter.com/!/DrEbraheim_UTMC
Find me on Instagram @OrthoInitiative

ABDOMINAL COMPARTMENT SYNDROME // Causes, Types, Clinical Features, Management
Subtitles (closed captions) are available for this video.
……………………..
Try to answer the following questions after watching this video.
(1) How is abdominal compartment syndrome (ACS) categorized?
(2) What causes primary/acute abdominal compartment syndrome (ACS)?
(3) What are the cardinal signs of abdominal compartment syndrome?
(4) How is intraabdominal pressure (IAP) measured in the workup of abdominal compartment syndrome (ACS)?
(5) How is abdominal compartment syndrome (ACS) graded based on intraabdominal pressure (IAP) measurement?
(6) What is the most dangerous complication occur during the treatment of abdominal compartment syndrome (ACS)?
(7) Which medications are used in the treatment of Abdominal Compartment Syndrome?
……………………..
Find out more videos at https://www.youtube.com/channel/UCICMHbwtxtj3ub05Jko1N_w
DISCLAIMER: The information provided in this video is intended SOLELY for educational purpose ONLY.
All of your feedback and advice are greatly appreciated!
SLEEP IS FOR THE WEAK
abdominalcompartmentsyndrome emergencymedicine reperfusionsyndrome roundbellysign trauma sleepisfortheweak intraabdominalpressure
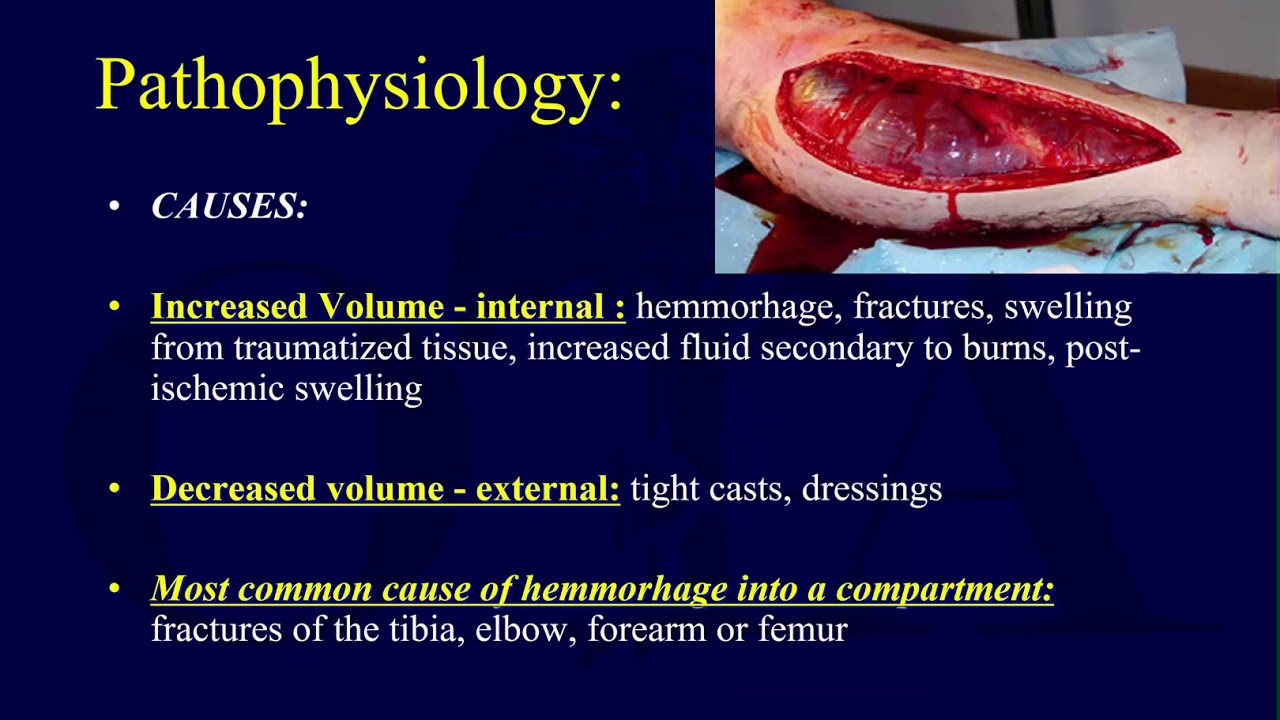
Compartment syndrome 1 – pathophysiology (OTA lecture series III g04a)
Narrated, annotated lecture 1 of 3 on compartment syndrome from the OTA resident lecture series (narrated by Saqib Rehman, MD), from Orthoclips.com.
Compartment Syndrome Animation – Everything You Need to Know – Dr. Nabil Ebraheim
Dr. Ebraheim’s educational animated video describes in detail the anatomy relevant to compartment syndrome.
Compartment Syndrome is a condition in which increased pressure in an enclosed space compromises the circulation of the tissues contained within that space. This condition can affect any compartment in the body. But, it most often involves the lower leg. Almost any injury can cause this syndrome, including injury resulting from vigorous exercise. However, the most common causes of compartment syndrome are fractures and soft tissue injuries. In this specific example, the tibia has suffered an oblique fracture from a traumatic force. Adema and hemorrhage caused fluid accumulation, elevating the compartmental pressure and occluding blood vessels and nerves. With clinical suspicion of acute compartment syndrome, inter compartmental pressure is measured. An absolute pressure of 30mmHg or higher or within 30mmHG of the diastolic blood pressure is considered diagnostic of acute compartment syndrome. Without urgent decompression, tissue ischemia, necrosis, and functional impairment will occur. Anatomy is crucial in the treatment of compartment syndrome. The four compartments of the leg include: The anterior, lateral, superficial, and the superficial and deep posterior compartments.
Fasciotomy is the treatment of choice for compartment syndrome. Complete decompression of the lower leg is accomplished through a double incision for compartment fasciotomy. The first incision is placed halfway between the fibula shaft and the tibial crest. The fascia anterior and posterior to the septum is opened transversely. The anterior compartment is released first, followed by the release of the lateral compartment.
Care should be taken not to injure the superficial peroneal nerve, located within the lateral compartment. The second incision is made medial to the previous incision, two centimeters posterior to the posterior tibial margin. Care should be taken not to injure the saphenous nerve and vein. The fascia anterior and posterior to the septum is open transversely. The superficial posterior compartment is released first, followed by the release of the deep posterior compartment. The double incision for compartment fasciotomy is now complete. Chronic exertional compartment syndrome is an exercise induced condition, different from acute compartment syndrome. In patients with chronic exertional compartment syndrome, the resting inter compartmental pressure is usually greater than 15mmHg. Pressure rises steeply after initiation of exercise, usually culminating in pain within 20 minutes. Burning, cramping, or aching pain and tightness develop leading to a cessation of activity. Intra compartmental pressure that remains over 30mmHg one minute after the end of exercise or pressure that remains over 20mmHg for longer than 5 minutes after the end of exercise is considered diagnostic of chronic exertional compartment syndrome. While initial treatment is conservative, a fasciotomy is the only proven successful treatment

Compartment Syndrome,Diagnosis,Pressures,Fasciotomy- Everything You Need To Know- Dr. Nabil Ebraheim
Educational video describing pressure measurement and fasciotomy.
A traumatic injury, such as a fracture of one of the long bones in the body (tibia), can often trigger acute compartment syndrome. The patient will complain of severe pain and narcotic requirements are usually increased. The trauma from injury or surgery will cause the limb to continue to swell. The cast is dressing will need to be removed so the limb can be inspected to rule out the presence of impending compartment syndrome.
Inspection and examination for the signs and symptoms of compartment syndrome should be done early and carefully. If the patient has swelling, pain and pain with passive stretch more than expected from the injury or surgery there is high probability that the patient is developing compartment syndrome.
Do not wait for all 5 P’s to appear, as these findings are considered ate findings:
•Pain/swelling
•Pulselessness
•Paresthesia
•Pallor
•Paralysis
If compartment syndrome is suspected, compartment pressure should be measured. If the pressure exceeds 30 mmHg or within 30 mmHg form the diastolic pressure, immediate fasciotomy is necessary.
The intracompartmental pressure of 30 mmHg is the generally accepted value for diagnosis. Opposing values have been suggested.
Relative pressure (perfusion pressure gradient)
P = diastolic blood pressure intracompartmental pressure.
Decompression of the involved compartments is indicated if the P falls to under 30 mmHg.
The value of the diastolic blood pressure in a patient under anesthesia with suspected compartment syndromes questionable. Do not rely on these values to get accurate information of the p. DBP under anesthesia is usually less.
Location of pressure monitor insertion is based on the etiology. A localize injury, especially a fracture, creates pressure gradient in the surrounding tissue that peaks within 5 cm of the injury. Intracompartmental pressure should be taken within this range to avoid misdiagnosis. Vascular injury and repair lead to reperfusion edema in the entire area of ischemia. The pressure gradient around the injury is therefore more diffuse, so the location of the needle insertion does not have to be as exact for the fracture or trauma.
Diagnosis: measuring the pressure is the most reliable method to confirm clinical diagnosis of compartment syndrome.. it is the most important step in establishing the presence of an early or impending compartment syndrome. Once the diagnosis is made, urgent fasciotomy should be done.
Solid state transducer intracompartmental catheter:
1Turn device on
2Attach the diaphragm chamber and 18 gm side ported needle to syringe.
3Place the needlesyringe assembly into the STIC motor unit
4Close cover of the unit.
5Slowly depress the plunger to remove any air from diaphragm and needle.
6Hold unit in direction of insertion and press zero
7Mark and prep area where STIC is to enter the compartment
8Inject local anesthesia
9Gently insert STIC needle
10Inject 0.3 cc saline to equalize the interstitial pressure
11Once pressure come to equilibrium, the pressure may be read from the monitor.
The most common compartment test for compartment syndrome of the leg is the anterior tibial compartment.
The anterolateral incision is placed halfway between the fibular shaft and the tibial crest.
The posteromedial incision is placed 2 cm posterior to the posterior margin of the tibia.
Become a friend on facebook:
http://www.facebook.com/drebraheim
Follow me on twitter:
https://twitter.com/!/DrEbraheim_UTMC

นอกจากการดูหัวข้อนี้แล้ว คุณยังสามารถเข้าถึงบทวิจารณ์ดีๆ อื่นๆ อีกมากมายได้ที่นี่: ดูวิธีอื่นๆGENERAL NEWS
Articles compiled by CASTU. See more articles in category: GENERAL NEWS

