You are viewing this post: Intramedullary Nailing of Right Femur Fracture | closed fracture femur คือ
Table of Contents
Intramedullary Nailing of Right Femur Fracture
นอกจากการดูบทความนี้แล้ว คุณยังสามารถดูข้อมูลที่เป็นประโยชน์อื่นๆ อีกมากมายที่เราให้ไว้ที่นี่: ดูความรู้เพิ่มเติมที่นี่
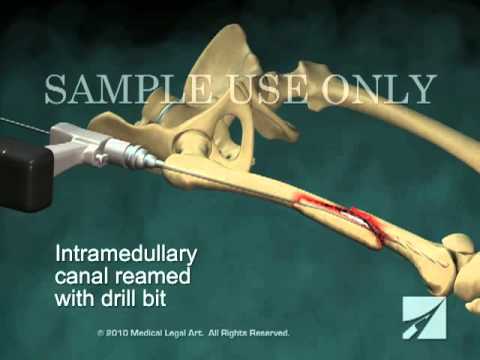
This 3D medical animation features a dramatic surgical overview during the operative placement of an intramedullary nail into the right leg to secure a comminuted femur fracture.\r
\r
Item ANS00126
Femoral Neck Fracture Nonunion – Everything You Need To Know – Dr. Nabil Ebraheim
Dr. Ebraheim’s educational animated video describes femoral neck fracture nonunion.
Follow me on twitter:
https://twitter.com/!/DrEbraheim_UTMC
Femoral Neck Fracture Nonunion
Femoral neck fracture nonunion has multiple facets and is important to understand all aspects of this important problem.
Example:
40 year old patient had a displaced femoral neck fracture, fixed with multiple cancellous screws about 9 months ago. The patient still has persistent groin pain. The patient cannot bear full weight on the hip. The patient has a painful limb, antalgic gait, and difficulty in walking. Xrays are not clear and show a possible nonunion. CT scan shows the nonunion with some Varus angulation. The treatment for this would be removal of the hardware and valgus osteotomy.
The scenario can be more complicated by adding a healed femoral shaft fracture to the nonunion of the femoral neck. In this case, you will do removal of the hardware from the femur and removal of the screws from the femoral neck nonunion. You will do valgus osteotomy and fixation with a plate, preferably a blade plate, to treat the nonunion of the femoral neck.
Intracapsular fractures of the proximal part of the femur are not common in adults younger than 50 years old, but they are associated with a high incidence of avascular necrosis and nonunion. About 1030 % of femoral neck fractures go to nonunion after ORIF. It is usually the vertical fracture pattern, such as Type III in Pauwels Classification. These fractures are more prone to nonunion due to shear stress, rather than compression forces across the fracture site. In Garden Classification fracture Type IV, where the fracture is completely displaced, the greater the displacement, the higher the incidence of nonunion and reoperation rate after fixation of the femoral neck. The inverted triangle pattern of fixation of femoral neck fractures is the one that is commonly used with the inferior screw posterior to the midline and adjacent to the calcar. Achieving and maintaining anatomic reduction is important for femoral neck fracture fixation and healing. The femoral neck fractures are intracapsular. There will be no abundant callus formation during the healing (healing is intraosseous only). Sometimes it is difficult to know if the fracture healed or not. There is no correlation between age, gender, and rate of nonunion. Varus malreduction correlates with failure of fixation after reduction and cannulated screw fixation. Posterior comminution of the fracture does not allow stable fixation and can lead to nonunion. The comminution of the femoral neck is usually posteriorly and inferiorly. Some recommend adding a fourth screw in this situation. High energy fractures have a worse prognosis for healing, especially in patients with metabolic bone disease and nutritional deficiency. When you see a femoral neck nonunion after fixation, you need to get blood work and rule out infection (get sedimentation rate and CRP). For the high angle femoral neck fracture, follow the patient up closely with clinical exam and xrays. There might be a Varus collapse on the xrays. You may see a femoral neck nonunion or a failed internal fixation. The patient walks with a limp, the limb is shortened, and the patient may have rotational deformity of the extremity. In the young patient with a femoral neck nonunion, arthroplasty is not a desirable option. In a young patient with femoral neck fracture nonunion, valgus intertrochanteric osteotomy with plate fixation produces a good result in the majority of cases. Valgus intertrochanteric osteotomy with plate fixation produces approximately 80% union rate and the procedure makes a vertical fracture more horizontal, converting the shear forces into compressive forces. It is done in a healthy, young patient with no joint arthritis and when the femoral head is intact. This procedure also corrects the Varus malalignment. Basically, the procedure changes the vertical fracture orientation to a horizontal fracture to achieve compression. Other procedures done in the young patient include revision ORIF with or without bone graft, but this is rarely done. Other procedures done in the young patient also include free vascularized fibular graft which is done in some patients especially in the younger patient with a nonviable femoral head. Hemiarthroplasy is done in patients with low physical demands. The articular cartilage of the patient is preserved with no evidence of infection. Total hip arthroplasty is done in patients that are older, in patients that have hip arthritis, if the femoral head is not viable, or if the hardware is cut out. It can also be done in younger patients that are active, when the femoral head is not viable and the patient does not want a free vascularized fibular graft or if the patient had collapse of the femoral head with nonunion. The problem with total hip replacement in this situation is more dislocations of the hip postoperatively.

Fracture Femur Types – Everything You Need To Know – Dr. Nabil Ebraheim
Dr. Ebraheim’s educational animated video describes the types of Femur Fractures according to location, Proximal, Diaphysis, Distal.

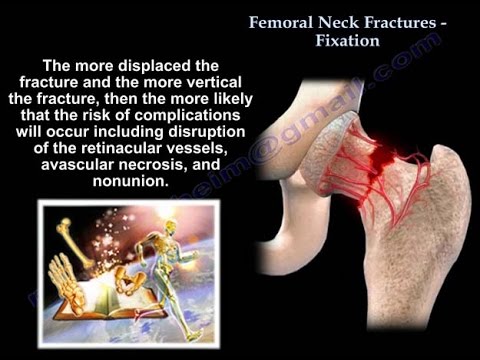
Femoral Neck Fractures Fixation – Everything You Need To Know – Dr. Nabil Ebraheim
Dr. Ebraheim’s educational animated video describes femoral neck fracture fixation.
Anatomy : The neck shift angle is approximately 130°. Anteversion is approximately 10°. No periosteum in the femoral neck and no abundant callus. The fracture heals by endosteal proliferation. The medial femoral circumflex is the most important blood supply to the femoral head (lateral epiphyseal artery). In young patients, injury is usually high energy that may lead to avascular necrosis. Some believe that surgery should be urgent in the young patient in order to decompress the compressed vessels. The more displaced the fracture and the more vertical the fracture, then the more likely that the risk of complications will occur including disruption of the retinacular vessels, avascular necrosis and nonunion. Femoral neck reduction should be anatomic, either by closed technique or open technique (if closed reduction technique fails).The calcar is an area of stress transfer. It is a posteomedial dense plate of bone. It forms an internal strut within the inferior portion of the femoral neck and intertrochanteric area.
Mechanism of Injury: Low energy fracture occurs in the elderly from a fall onto the greater trochanter. A fall in the elderly is different than a fall in the young. The older patient has less protective reflexes during a fall. The younger patient has better protective reflexes during a fall. Wrist fractures occur in the younger group than fractures of the hip. The young will try to protect themselves by falling on the wrist. High energy fractures can occur in the young or the elderly from either a fall or a car accident. Stress fractures can occur in athletes. Insufficiency fracture in the elderly (occult).
History: Obtain adequate history from the patient such as any syncopal episodes and loss of consciousness. The preinjury ambulatory status may determine the treatment selected for the patient. Falls and low sodium will increase the risk of hip fractures.
Clinical Exam: Position of leg is usually shortening and external rotation.
Patient Mortality: 1 year mortality rate is approximately 30%. Surgery delay more than 4 days may double the mortality rates (these patients are probably sicker than the average patient). Medical comorbidities (4 or more increases mortality). Renal patients with hip fractures are a problem. Institutionalized patients and low sodium levels may also be risk factors.
Surgical Timing: The optimal time for surgery is after medical stabilization. There is an improved outcome if surgery is done within 48 hours. Surgical delay up to 72 hours for medicals stabilization is warranted in unhealthy patients.
Surgery: Displacement and physiological age of the patient will decide the treatment. Nondisplaced fractures should be fixed to prevent displacement. This is done for the young and older patients and it is a minimal surgery. Screws are placed in an inverted triangular pattern with inferior screws posterior to the midline and adjacent to the calcar. If the fracture is displaced and the patient is young, you will do closed reduction or open reduction to have the fracture be anatomic (reduction of the fracture should be anatomic). Avoid malreduction! Adequacy of reduction is the most important factor. A healed femoral neck fracture with shortening is associated with a poor functional outcome.
Treatment: Treatment for a displaced fracture in active elderly patients will be a total hip replacement. It is also used in patients with degenerative arthritis or rheumatoid arthritis and femoral neck fractures. Treatment for a displaced fracture in debilitated, inactive elderly patients will be a bipolar or unipolar hip replacement.
Surgery for Nonunion: Valgus Intertrochanteric Osteotomy in the young will change the orientation of the fracture from vertical (biomechanically bad) to horizontal (biomechanically good).
Follow me on twitter:
https://twitter.com/!/DrEbraheim_UTMC
Donate to the University of Toledo Foundation Department of Orthopaedic Surgery Endowed Chair Fund:
https://www.utfoundation.org/foundation/home/Give_Online.aspx?sig=29
Femur Fracture, Periprosthetic fracture – Everything You Need To Know – Dr. Nabil Ebraheim
Dr. Ebraheim’s educational animated video describes the periporsthetic fracture of the femur in a simple and easy way.
Vancouver classification for postoperative periosteopathic femur fractures.
Fractures around the total hip prosthesis are occurring more frequently. Vancouver classification is the most classification used (very popular on exam). Vancouver classification relies on the level of the fractures, if the prosthesis is stable or not and the quality of the bone.
Vancouver classification is
(A) Proximal femur trochanteric area
(B) Fracture occurs at or near the distal tip of the hip prosthesis.
(C) Occurs well below the hip prosthesis
Type Ag
•Proximal femur greater trochanteric area.
•Fractures in the trochanteric region can be stable and can usually be treated conservatively.
•If the fracture is migrated 2.5 cm, it probably will need surgery.
•Do surgery for displacement of the fracture or instability of the prosthesis.
•Nonunion is associated with pain, instability, weak abduction and gait disturbances.
Type AL
•Fracture in the lesser trochanteric region.
•Usually symptomatic treatment
•Check stability of the prosthesis
•If substantial aspect of the medial part of the femur is included with the lesser trochanter, revision of the total hip arthroplasty with reconstruction of the medial buttress may be necessary.
Type (B)
•Fracture occurs at or near the distal tip of the hip prosthesis.
•There are three types:
Type B1: stable stem. B1 is associated with the most complications of all the fracture types because the fractures are usually unstable.
Type B1 treatment: ORIF using a cerclage cable or locking plate.
Type B2: loose stem, fracture occurs ar or near the distal tip of the hip prosthesis. It is very difficult to differentiate between type B1 and type B2 based on xrays alone.
Type B2 treatment: revision to long, porous, cementless stem.
Type B3: loose stem and proximal is poor quality or severely comminuted fracture.
Type B3: treatment: revision of the femoral component with proximal femoral allograft or proximal femoral replacement.
Type C
•occurs far below the hip prosthesis
•Type C treatment: ORIF with a plate.
If the physician can bypass a perforation utilizing a prosthesis that ends 23 femoral shaft diameters distal to the perforation, this will reduce the risk of fracturing through the perforation.
Become a friend on facebook:
http://www.facebook.com/drebraheim
Follow me on twitter:
https://twitter.com/!/DrEbraheim_UTMC
Background music provided as a free download from YouTube Audio Library.
Song Title: Every Step

นอกจากการดูหัวข้อนี้แล้ว คุณยังสามารถเข้าถึงบทวิจารณ์ดีๆ อื่นๆ อีกมากมายได้ที่นี่: ดูวิธีอื่นๆGENERAL NEWS
Articles compiled by CASTU. See more articles in category: GENERAL NEWS

